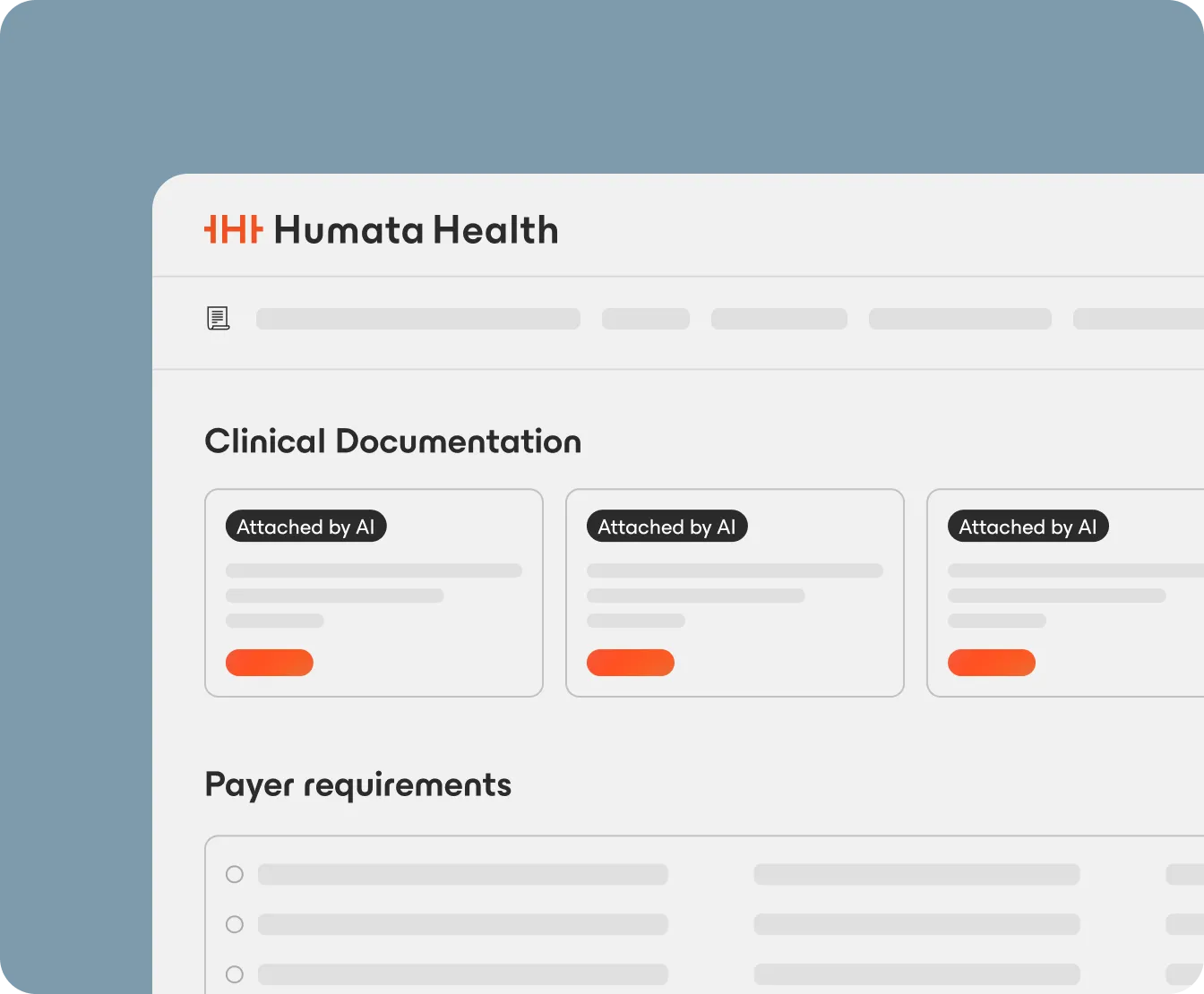
Humata automates the entire prior authorization process, from intake to decisioning to post-auth monitoring. Designed for providers and payers, our solution helps healthcare organizations accelerate care, reduce denials, and recover revenue.
Built for healthcare and trusted by leaders
























Humata's Frictionless Prior Authorization™ automates clinical review and transforms prior authorization—empowering health plans to drive consistency, reduce reviewer workload, and improve compliance.
Replace manual review with AI-powered summaries, streamlining nurse workflows and accelerating decisions.
Standardize submissions to meet payer requirements, driving faster and more consistent approvals.
Automation handles routine cases, escalating only outliers for clinical attention.
Structured, auditable processes minimize decision variability and fulfill CMS-0057 requirements.
First-pass approval rate

Improvement in clinical bundling efficiency

Less authorization touches

How does Humata integrate with our existing UM systems and data workflows?
Can Humata support multiple lines of business and payer-specific requirements?
What measurable efficiency and compliance outcomes can we expect?