Designed for providers and payers, our solution helps healthcare organizations accelerate care, reduce denials, and recover revenue.



What the numbers show
improvement in clinical bundling efficiency
time reclaimed from document work

first-pass approval rate
Time reclaimed from document work

reduction in write-offs

improvement in peer-to-peer

improvement in days-out
improvement in days-out

fewer reschedules

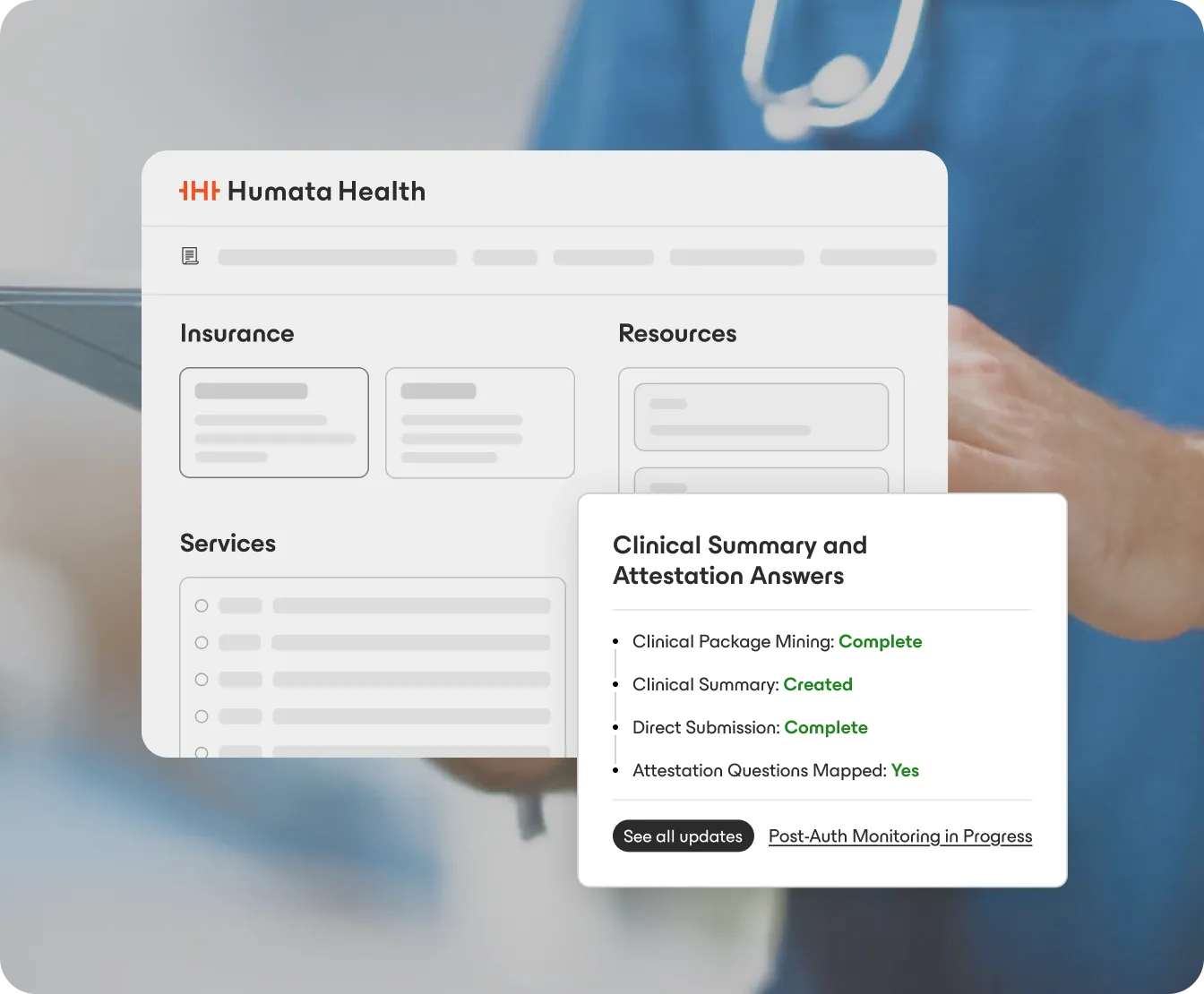
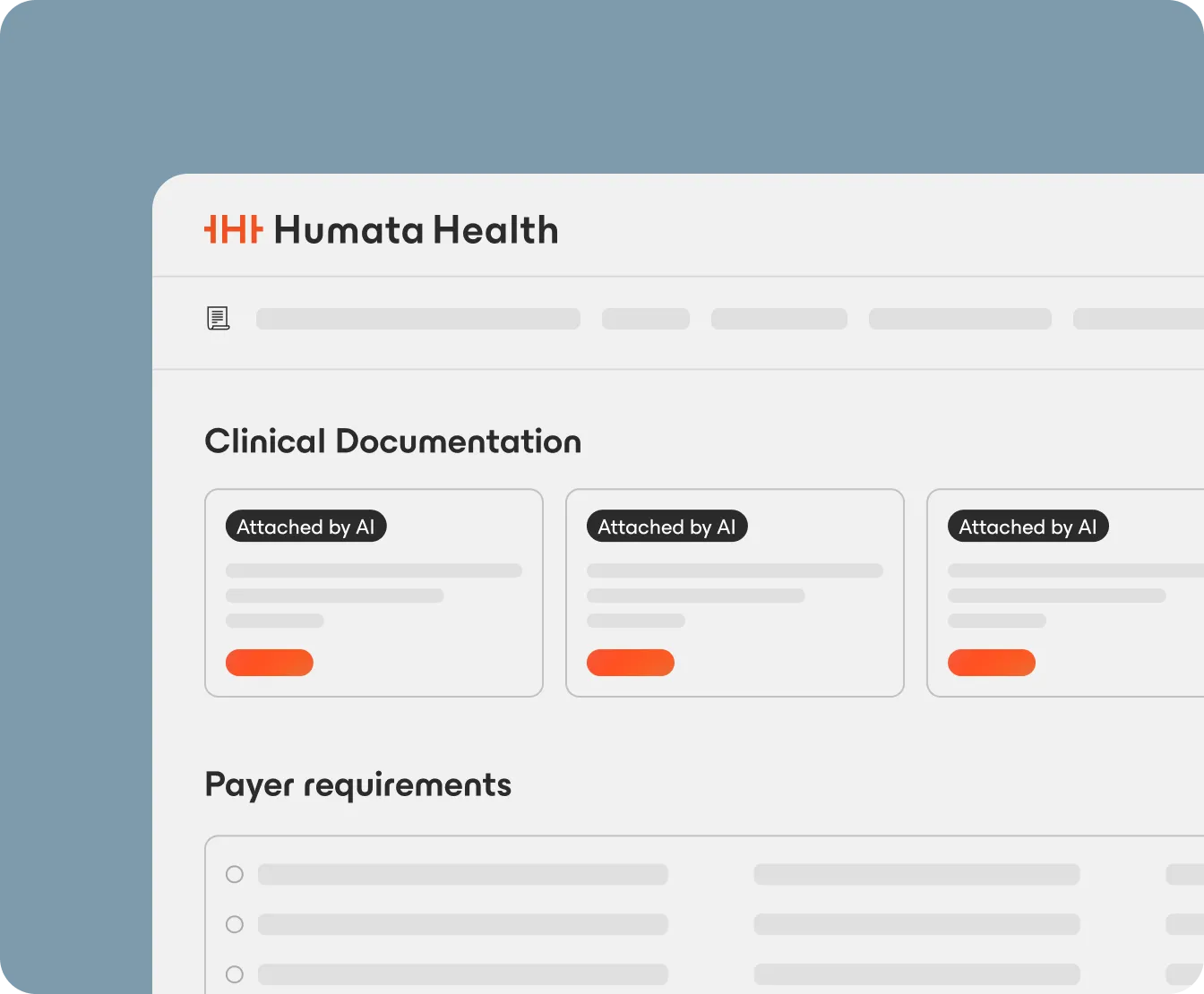
Our modular solution is designed to solve specific challenges within the prior authorization process, creating a comprehensive, end-to-end solution.


Our solution is powered by the largest and most robust partner ecosystem in the industry, ensuring seamless connectivity and deep integration with the systems you use every day.


.webp)


%201-1.webp)
250+ payer connections


.webp)


%201-1.webp)

250+ payer connections
Order Integration
Payer Interoperability
Appointment Integration
Automation, AI & Augmentation
Clinical Document Integration
eMPA Widget
Policy Integration
Analytics via Power BI





.webp)


%201-1.webp)

250+ payer connections

.webp)


%201-1.webp)
250+ payer connections
Order Integration
Payer Interoperability
Appointment Integration
Automation, AI & Augmentation
Clinical Document Integration
eMPA Widget
Policy Integration
Analytics via Power BI