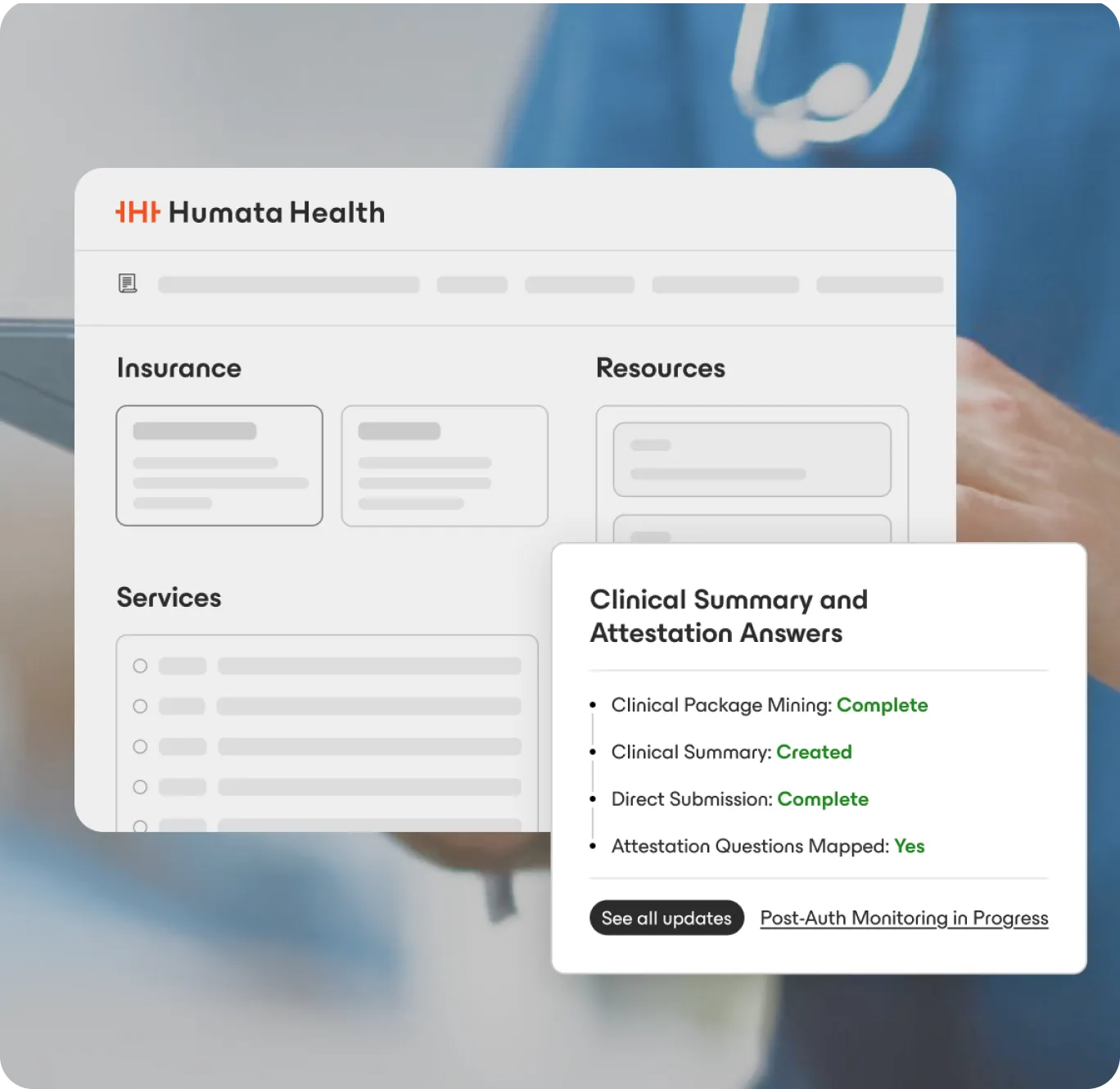
Humata streamlines drug authorizations by unifying medical and pharmacy benefits in one workflow—bundling clinicals, managing attestations, and verifying policies to reduce denials, recoupments, and delays.
Built for healthcare and trusted by leaders
























Humata's Frictionless Prior Authorization™ streamlines authorizations for specialty drugs and infusions, reducing denials, preventing rework, and keeping pharmacy, infusion, and billing teams in sync from order to administration.
Automate drug authorizations for medical and pharmacy benefits in one process.
Auto-bundle clinical data and complete attestation forms with evidence directly from the EHR.
Verify submissions against payer policies before sending to minimize denials, reviews, and recoupments.
Use automated updates and EHR write-backs to keep pharmacy, infusion, and billing teams in sync.
First-pass approval rate

Improvement in clinical bundling efficiency

Less authorization touches

How does Humata integrate with pharmacy, infusion, and billing systems—and handle medical vs. pharmacy benefit routing?
Can Humata support multiple lines of business and payer-specific requirements?
What measurable efficiency and compliance outcomes can we expect?
Continue Exploring
